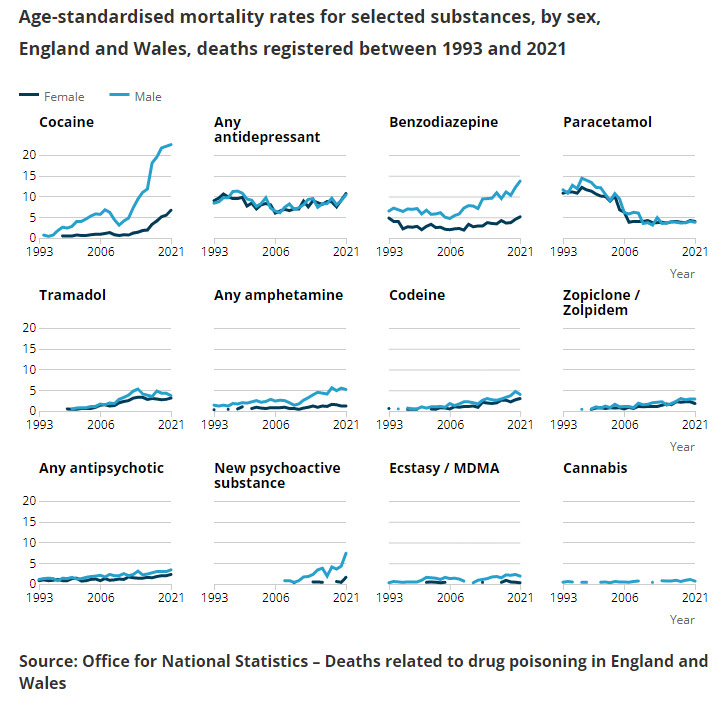
A particularly concerning trend has been flying under the radar for several years now – an increasing number of deaths from drug poisonings involve benzodiazepines, pregabalin, gabapentin or zopiclone.
Every year the Office for National Statistics shares new information on deaths related to drug poisoning in England and Wales. And every year, for almost a decade now, those figures demonstrate that the situation is getting worse. Since 2012 the number of people dying has been on a steadily upward trajectory, with 2021 seeing a record 4,859 deaths.
A particularly concerning trend has been flying under the radar for several years now – an increasing number of deaths from drug poisonings involve benzodiazepines, pregabalin, gabapentin or zopiclone.
When these drugs are implicated in deaths it is almost always (over 93%) alongside other substances, particularly opiates and alcohol.
But why the increase? Here, it may be instructive to look across the border.
In Scotland the situation has spiralled rapidly in the last decade, with almost three quarters of 2020 deaths involving benzodiazepines. This huge increase is largely due to increasing use of “street benzos” rather than the prescribed drugs with one, etizolam, implicated in almost two thirds of deaths in 2020. These drugs – cheaper, illegal and unregulated – can sometimes be 50 times as strong as a prescription benzodiazepine, substantially increasing the risk of harm to the person taking them.
Awareness – and worry – is growing in England too. In July 2020 Public Health England released a warning about evidence of harm from “illicit or fake benzodiazepines” and in and in May 2021 noted “most illicit benzodiazepines no longer contain the substances they are sold as”.
To discuss harms related to benzo use – and ways we can work together to reduce them – last month Collective Voice held a webinar with clinical and policy experts. A full recording of the webinar is available here.
We heard from:
- Dr Jeffrey Fehler, Consultant Psychiatrist, Central & North West London NHS Foundation Trust
Download Jeffrey’s presentation
- Steve Taylor, Programme Manager, Alcohol & Drugs Treatment & Recovery, Office for Health Improvement and Disparities
- Dr Roya Vaziri, Executive Medical Director, Humankind
So what did we conclude?
Firstly, there is a gap in up-to-date knowledge about the scale of use in England and Wales, particularly with respect to “street benzos”, because of the limits to drug testing. Surely we can do more than wait for trends to be picked up in briefings on people who have died? We need to better understand who is using benzodiazepines and why.
Secondly, there is a lack of awareness among people using drugs about the dangers of street benzos and polydrug use. We know there are multiple groups of people using benzos – so talking to them and listening to their stories will be vital in beginning to design effective ways to reduce harm.
Finally, there is a lack of evidence of ‘what works’ in supporting people who use benzos. However given “The Orange Book” is built not just on formal evidence but practitioner expert consensus perhaps it’s time as a field we use this approach to develop tailored guidance on benzos use?
Related Content
Collective Voice CYP Forum responds to ACMD drug prevention report
The report provides an excellent overview of the current drug prevention landscape in the UK. It’s comprehensive, evidence-led, and crucially draws operational insights from those currently delivering prevention activities.
Work as recovery: Supporting employment during Alcohol Awareness Week
This Alcohol Awareness Week, WithYou is calling on employers and policymakers to recognise work as a recovery tool, which can change the lives of people
Collective Voice responds to the 10-year health plan
When the plan trumpets ‘a devolved and diverse NHS’, I wonder if it should really be saying ‘ a devolved and diverse health system’ Read