The speech the Chancellor made on Wednesday made much of the (welcome) investment in the health service – £6 billion being made available in the first year of the Spending Review, and £600 million specifically to improve mental health services.
What wasn’t in the speech but emerged later was a decision to reduce the size of the public health grant by 3.9% a year for the rest of the Parliament. Those are cuts that will hit all of us delivering drug and alcohol services whether we’re in the Third Sector or in the NHS.
Collective Voice in our submission to the Spending Review, and in subsequent briefings, made it clear that reductions in the support for drug and alcohol treatment have consequences not only to the NHS but also to the police and criminal justice system.
For example, a recent Healthwatch England report on hospital discharge pointed out that homeless people (many of whom have substance misuse problems that are untreated) attend hospital as many as 30 times per year. They give this case study of what that means for our already overstretched Emergency Departments and Ambulance Services:
“A heroin addict was seen six separate times at A & E about an abscess in his groin. He was ‘treated’ every time, not admitted and was discharged in a confused state. Paramedics were called out and said that if he had been left he would have died within a couple of hours.”
Cuts to drug and alcohol treatment will see more people having to fall back on acute services with potentially tragic consequences.
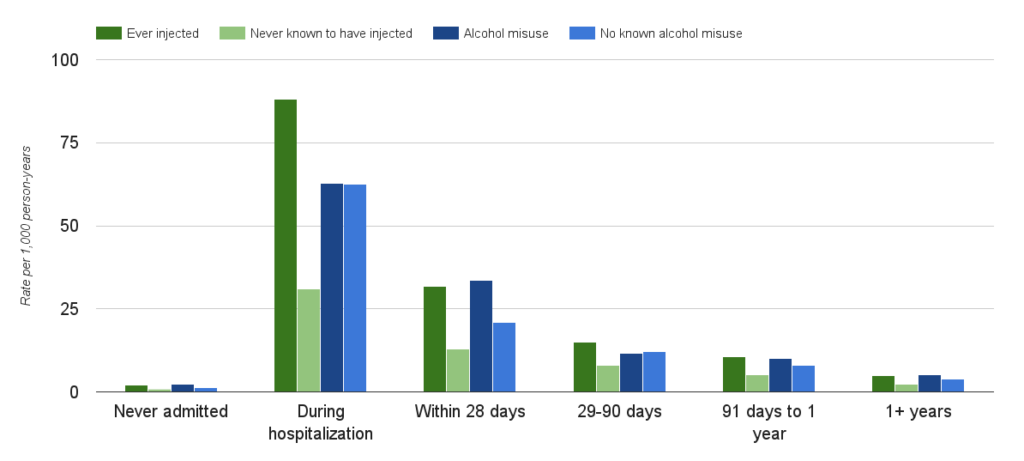 New research from Scotland suggests that, even for people in the substance misuse treatment system, being in hospital is a significant risk factor for dying.
New research from Scotland suggests that, even for people in the substance misuse treatment system, being in hospital is a significant risk factor for dying.
While the Spending Review has provided some (again welcome) protection to resources available to the police, the respected Police Foundation have been clear that cuts elsewhere will impact on their ability to keep us safe.
“Many of the pressures the police experience from non-crime demand will not go away. Big cuts to local government funding and the wider criminal justice system mean we need to reorganise the public service frontline to deal with problems such as high reoffending rates, child safeguarding and rising levels of mental illness.”
Data published by the Centre for Public Health about the Drug Intervention Programme in Merseyside continues to show that problematic drug use remains a driver of crime. Over half of the nearly 10,000 drug tests carried out in the region came back positive, with about 2,500 people testing positive for opiates.
Many of those people will have been diverted into drug treatment where, recently published research from Manchester University, suggests there will be an almost immediate impact on the level of crime and drug use of people entering treatment.
Whether that is sustainable over the course of a Parliament which will see 20% falls in the resources available to local areas to deliver these services remains to be seen.
We can’t second guess what decisions local Health and Wellbeing Boards will be making about the future of drug and alcohol services, but looking back over the period we’ve just been through it is clear that both drug and alcohol services have already been asked to do ‘more with less’.
The LGA in their briefing on the Spending Review made it clear that in their view we are now entering a period where salami slicing may not be sufficient.
“Councils will do everything they can to protect services but these reductions will inevitably impact on health outcomes. Councils will in some cases be forced to make a decision between different services.”
We genuinely welcome the additional funding available for mental health services and the commitment to work with NHS England on implementing the recommendations of the Mental Health Taskforce when their review is published next year.
We know how important mental health is to the people we support in drug and alcohol treatment, and as the ACMD have recently noted there is an ongoing challenge to improve the quality of mental health support available.
Wherever possible we will work with the NHS locally and nationally to improve outcomes in this area.
Related Content
Collective Voice responds to the 10-year health plan
When the plan trumpets ‘a devolved and diverse NHS’, I wonder if it should really be saying ‘ a devolved and diverse health system’ Read
Collective Voice responds to the Independent Sentencing Review
There’s lots to welcome for our field, but the Government should approach some recommendations with caution. It would be a mistake to develop solutions today
The Government’s serious approach to synthetic opioids is welcome, but it can do more to provide national leadership
The Government is asking local areas to develop local preparedness plans and submit them for it to review. We can reasonably ask: what is in